Government must commit to allocating funds for healthcare, health experts say
The treasury must reprioritise its spending to address the gaps in resources for healthcare facilities created by the US’s termination of financial aid when it makes a second attempt to table this year’s budget next week, experts say.
Minister of Finance Enoch Godongwana is set to present the budget to parliament on 12 March after being forced to postpone it on 19 February after the cabinet failed to agree on points of contention among the coalition government partners. Chief among them was a two percentage point increase in VAT from 15 to 17%.
A focus point of the speech will be how the minister proposes to supplement health funding after US President Donald Trump cut aid to South Africa over policy differences.
The US Agency for International Development (USAid) used to fund 44 health projects in the country and supported the President’s Emergency Plan for Aids (Pepfar) as well as TB treatment. For the current US financial year, R8 billion was allocated to South Africa.
Health experts are anticipating that Godongwana will make a commitment to allocating money to these services in the near future, if not immediately.
“We would expect that the government has factored in, and taken into consideration, the huge impact of the sudden termination of funding for the continuation of key services,” said human rights lawyer and founding director of the Health Justice Initiative Fatima Hassan.
According to the budget proposals which were released to the media last month, but which Godongwana was not able to table before parliament, after his speech was cancelled, the total infrastructure allocation for health would have been R37.4 billion over the mid-term economic framework period.
While the government might not have been able to find the money in the time between 19 February and the permanent termination of USAid on 27 February, there needs to be some consideration for interim funding for “this year at least”, Hassan said.
“At the very least, we would expect that there’s an appreciation of the dire, not just financial impact, but the human impact of what this means for South Africa and that, embedded within the budget planning, is a plan for how [treasury] is going to mitigate the impact of the termination to ensure that, at a minimum, there is no interruption to the set of services and programmes that were being provided by US funding,” she added.
Around 5.8 million South Africans are on antiretroviral medication for HIV, and of those, 5.417 million are patients at public health facilities. About 1.6 million of these public sector patients — or around 30% — get their medicine for three months at a time, according to data from the health department.
One of the immediate effects of the termination of funding has been massive job cuts, affecting clinicians; counsellors; data capturers and collectors; researchers and community health workers at a number of mainly HIV/Aids organisations and treatment centres.
The Wits Reproductive Health Institute, Broadreach Healthcare, the Anova Health Institute and Right to Care were some of the HIV/Aids organisations that would no longer be funded, the Bhekisisa Centre for Health Journalism reported.
One clinician who spoke to the Mail & Guardian on condition of anonymity said the HIV/Aids NGO she works for, which was funded by Pepfar, has had to let go 2 800 workers after aid was cut. It has only managed to retain 5% of its staff.
Because of this, there were not enough staff to attend to patients.
“When you look at treatment, care and support — the actual staff on the ground who are helping people to stay in the service and to take their medicines correctly — 40% of that was funded by Pepfar,” she said.
“It’s all very well and good to say, ‘We’ve got the medicines; we’re on top of the programme,’ but what they’re not acknowledging is that you actually need that human connection at the facility to help people sustain their treatment commitment over a lifelong journey.
“Even with all of the Pepfar input, we were still struggling with loss to follow-up.”
The estimated number of job cuts as a result of the termination of funding is between 14 000 and 17 000, according to Shabir Madhi, the dean of the faculty of health sciences and a professor of vaccinology at the University of the Witwatersrand.
“In the current economic situation, [the job losses] are less than ideal and, when one person is unemployed, it means the whole family that’s dependent on that person obviously has consequences,” Madhi told the M&G.
The government would need to cut back on some spending to plug the gap left by the funding cuts but that might be to the detriment of other sectors, he added.
“I don’t foresee the fiscus being able to provide an additional R8 billion specifically for the HIV/TB programme. It’s already a big component of what is included in the health budget and such an increase [obviously needs] to come at the cost of cutting back on something else, rather than investment.
“The worst thing that can happen right now is for there to be cutbacks, which is already occurring, unfortunately, in terms of the number of doctors, the number of nurses that have been employed by provincial authorities.”
A survey conducted by the TB Community Coordination Hub found that more than half of 180 respondents from 31 countries said that their ability to deliver TB services has been “severely” impacted by the US stop-work orders, with nearly 25% having to close down their offices and projects entirely.
“I don’t believe that there isn’t money in the department of health programme. It’s about being efficient in terms of how the money is actually allocated and spent and minimising corruption,” Madhi said.
“If we can do that, there’s no reason why we shouldn’t be able to fill this gap and I think we need to have an honest discussion that we are in an upper-middle-income country, and most upper-middle-income countries will be taking responsibility for providing healthcare services to their public.”
Non-profit organisation Ibis Reproductive Health said it was concerned about the negative effect of the funding cuts on pregnant women or those seeking abortions.
“Many people already face barriers to accessing sexual and reproductive healthcare and the withdrawal of US government funding, including from the UN Population Fund, puts programmes at risk [which are] striving to improve access to maternal and sexual and reproductive healthcare,” its senior communications manager Duduetsang Mmeti said.
The department of health is “communicating with the treasury on a number of health programmes including the impact of the funding freeze”, spokesperson Foster Mohale said.
Without providing details, Mohale told the M&G that the department presented its “needs to sustain healthcare provision in the country, for consideration in terms of possible additional budget allocations”.
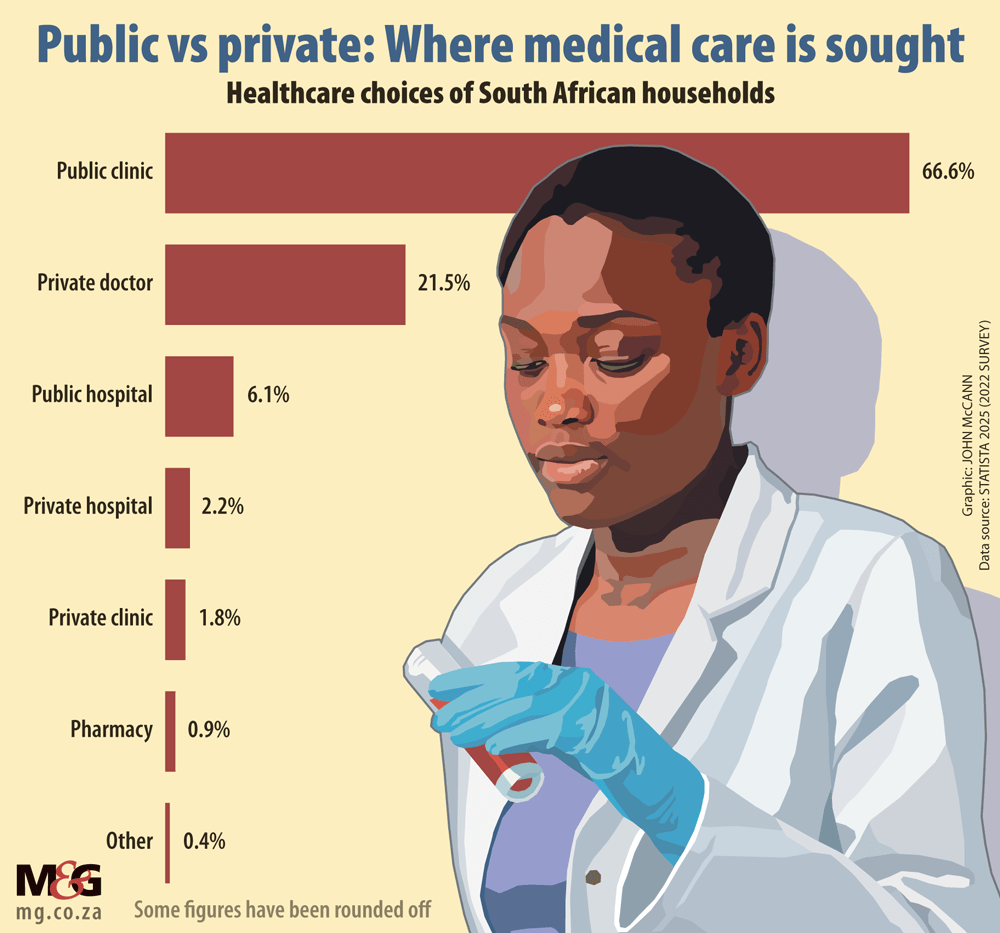
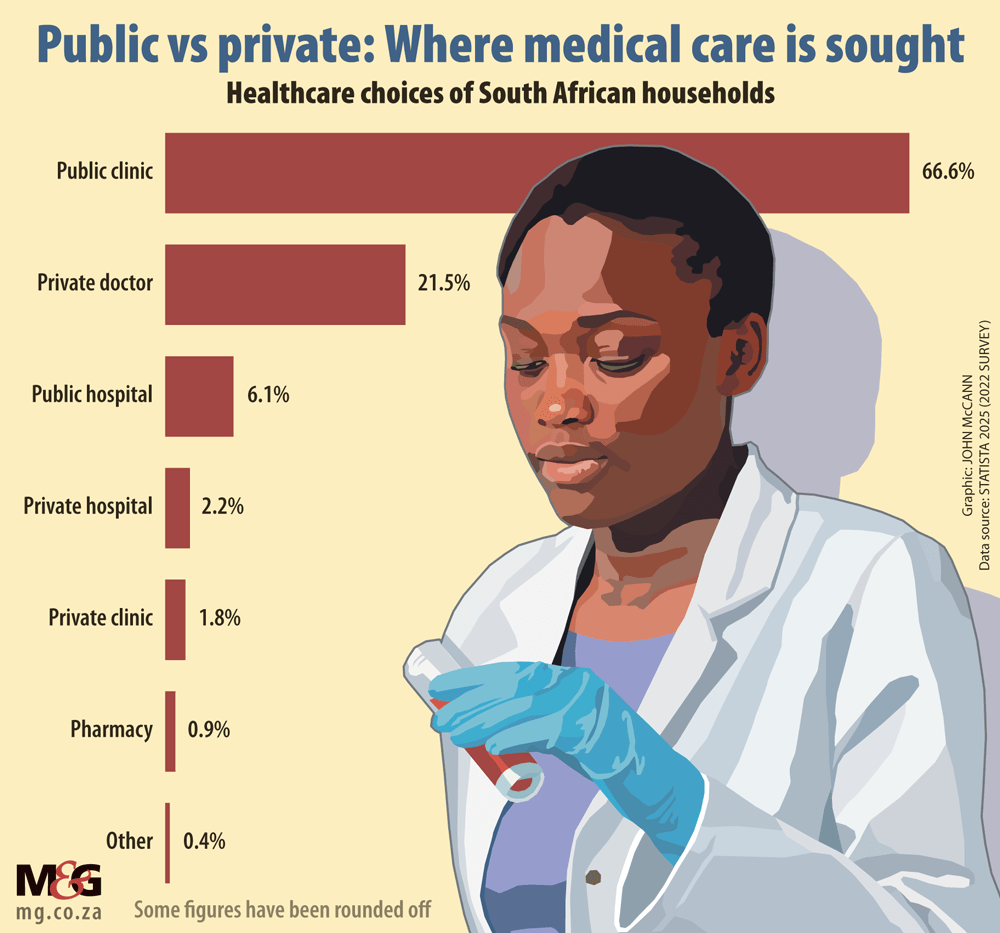
Given the size of the population that is reliant on the public health system, “there will never be enough of a budget”.
The government needs to show commitment to alleviating the pressure and burden on South Africa’s healthcare system, Hassan said.
“[We need to know] if there is a commitment to trying to find, on an expedited basis, the necessary resources to make sure that the minimum package of services and stuff that’s already been provided is not taken out of the system as a result of these cuts,” she said.
The conversation should lean towards where the government is going to find billions to maintain the healthcare and support services that are already being provided, so the country doesn’t roll back on the gains that have been made.
While there was no immediate risk of a surge in HIV/Aids cases, Madhi said the government needed to be proactive in addressing the gaps that have emerged, including in active screening programmes and testing and early treatment.
Failing that, South Africa might see a “reversal of the rates of HIV transmission in that it is going to start going up again in the medium term, in a period of perhaps five to 10 years”, he warned.




